05:12
People hope the COVID-19 outbreak will come to an end as soon as possible. So what could be in store for the epidemic? We don't have a crystal ball to show us the future, but we can get some clues from the past.
Both SARS and the virus that caused COVID-19 are known as coronaviruses, so it might be helpful to compare the 2003 SARS outbreak with the current one. This might present us with the best-case scenario, where the virus is put under control through public health intervention.
The best way to contain the virus in both outbreaks is to identify cases as soon as possible and put the infected in isolation.
In both cases, large-scale control measures were carried out. In 2003, the SARS outbreak ended in China after about six months. And it was eradicated worldwide after infecting over 8,000 people, and killing almost 800.
In addition, some scientists argued that the warm, humid weather of early summer greatly contributed to the fight against SARS. The same argument is being made about COVID-19.
But the new coronavirus is more cunning. The latest research shows that its spike protein design allows it to hold its grip over a cell 10 to 20 times more firmly than SARS. That explains why the new coronavirus is more infectious than SARS. It also has an incubation period of potentially more than 20 days, much longer than that of SARS. All this suggests that containing it is much harder.
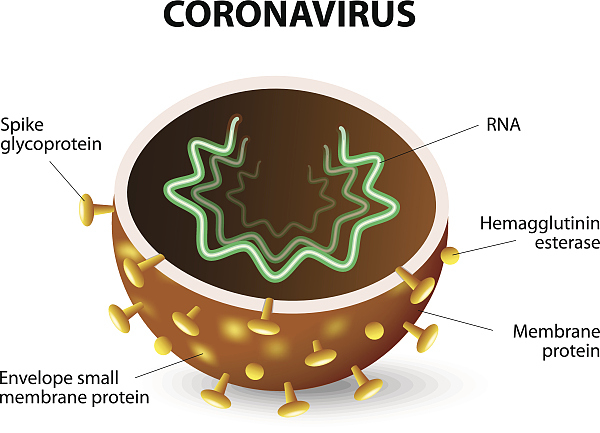
But this doesn't mean it is a patient virus. It has to move fast because its single strand nucleic acid structure is so fragile that it could be easily torn apart by powerful immune systems. It, therefore, causes acute symptoms in the host in order to swiftly leave and jump to another, infecting as many people as possible in a shorter period of time. But at the same time, this strategy sounds alarm for humans to trigger more measures to fight against it.
That's why SARS fizzled out so quickly and completely. Actually, there have been just three cases after 2004, all due to a lab leak. So, what happened to SARS? Where did it go? Scientists believe that the novel coronavirus was hidden in its natural host, the bat. In 2017, in a remote cave in Yunnan Province, virologists identified a single population of horseshoe bats. They harbor virus strains with all the genetic building blocks of the one that jumped to humans in 2003.
Furthermore, the government strictly banned the middle reservoir between bat and human, the civet, after the outbreak, preventing SARS from crossing the line. That could explain why MERS is still haunting humans in Middle East. The middle reservoir, the camel, is a major part of the local life in parts of the region. But, we still have no idea about the middle reservoir of the new coronavirus.
Another ending for an epidemic is what has been called "burn out." That's what happened to the Zika virus epidemic that hit South America between 2015 and 2016. Since Zika cannot infect the same person twice, thanks to the antibodies generated by the immune system, the epidemic reaches a stage where there are too few people left to infect for transmission to be sustained, just like fire flames consuming all the oxygen in a room and extinguishing itself. This is not a desirable scenario because it will cause more infections and deaths.
The last possibility paints a future in which the virus is not contained. The 2009 H1N1 pandemic virus could not be contained in the U.S. and therefore spread all across the world. Since then, this virus has circulated as seasonal flu. Evolution will enable the virus to find a balance between virulence and transmission. Many viruses, like HIV, will take on a milder form, trading off for wider spread. If that is the case, the new coronavirus may return seasonally and join the milder coronavirus strains that infect people as a common cold or pneumonia.