
"Nurses are the backbone of any health system," WHO Director-General Tedros Adhanom Ghebreyesus said on Tuesday, which marks this year's World Health Day. "Today, many nurses find themselves on the frontline in the battle against COVID-19."
However, nurses and other medical staff are facing great challenges and difficulties on the battlefield against the pandemic, which the director-general called on the whole world to "ensure they get the support they need to keep the world healthy."
Risking themselves as they save others
In China, a total of 42,000 medics from across the country were sent to Wuhan since the outbreak, which played an important role in the prevention and control of the epidemic, according to National Health Commission (NHC).
Among them 28,600 are nurses, accounting for 68 percent of the total number. "There is an old saying in China that in curing a patient, treatment contributes 30 percent while nursing is 70 percent," said Guo Yanhong, deputy head of the NHC's Medical Administration Bureau.
"Nurses are there, from temporary hospitals to isolated wards. Together with doctors, they have made positive contributions to saving patients' lives and reducing the case fatality rate," she said.
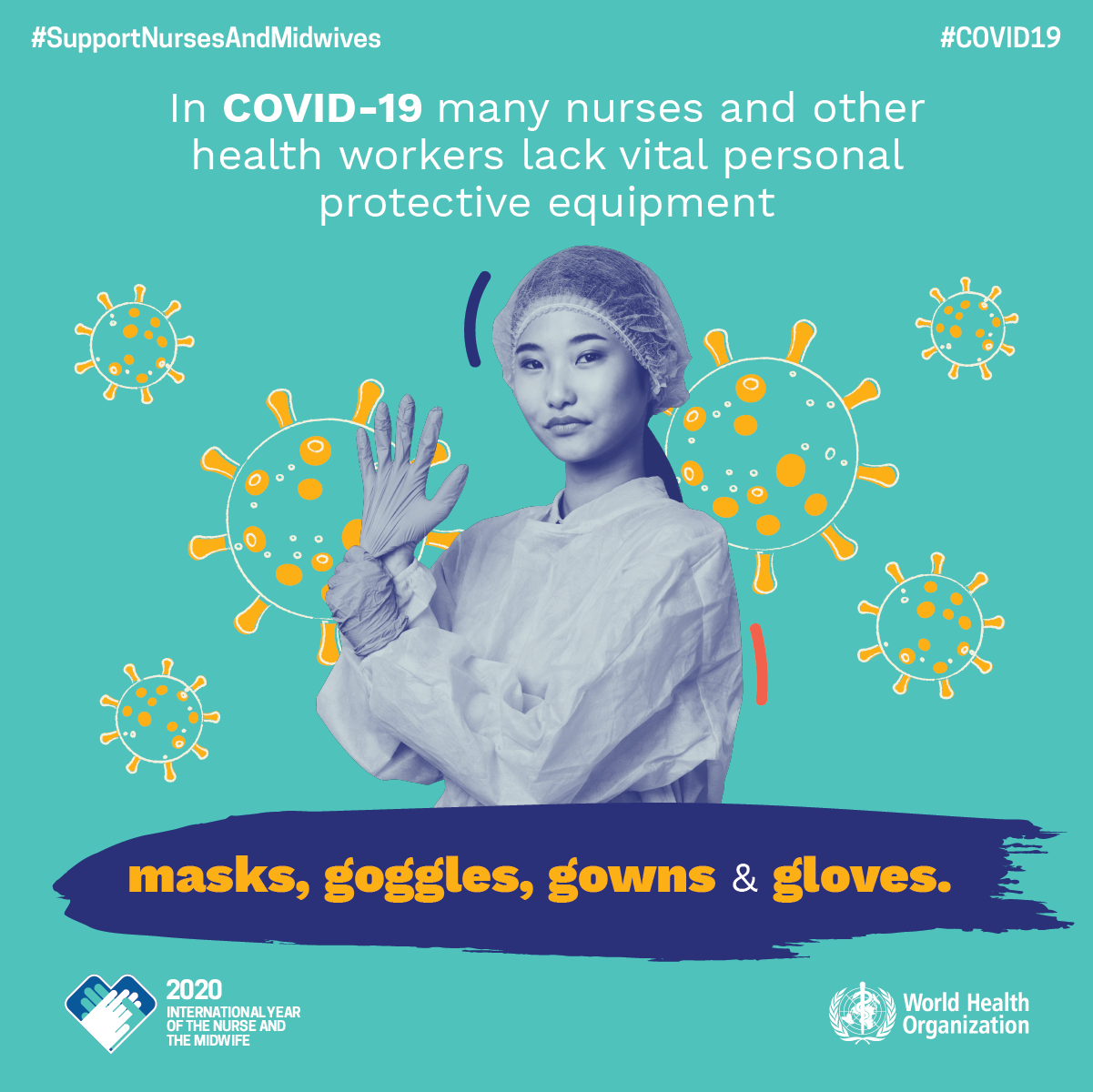
A WHO poster on World Health Day. /WHO
A WHO poster on World Health Day. /WHO
Behind the contributions is sacrifice.
Health care workers are at high risk of infection around the world due to lack of protective equipment.
According to a national survey made by the U.S. Department of Health and Human Services (HHS) from March 23 to March 27, the most significant challenges for 323 hospitals across the U.S. was testing and caring for patients with COVID-19 and keeping staff safe.
These hospitals reported that "widespread shortages of personal protective equipment (PPE) put staff and patients at risk," with the most commonly needed PPE items to be "masks (including N95 masks, surgical masks, and face shields), followed by gowns and gloves."
"There's nothing else to lose but our lives," said Diana Torres, a registered nurse at Mount Sinai West Hospital where they saw the first nurse known to die of COVID-19 in the New York City.
"I absolutely believe that he contracted this because of the lack of PPE in his unit and at his hospital – but that's across our nation," the sister of the deceased nurse told NBC News, hoping changes will be made to prevent other medics from suffering the same fate.
There are also reports of nurses quitting because they are unable to wear masks to protect themselves, or were threatened termination if they spoke out of the lack of PPE.
Read more: U.S. nurse quits after hospital says no wearing masks
Similarly, frontline medics in the UK reported they are being "bullied and shamed" into treating COVID-19 patients without having PPE, according to The Guardian.
Some are even told to "hold their breath" to avoid infection, which is "heartbreaking", Dr Samantha Batt-Rawden, president of the Doctors' Association UK (DAUK), told The Guardian. "Lack of personal protective equipment continues to be a critical issue…Doctors are dying. Nurses are dying. We are devastated, and can no longer stand by and watch as more dedicated colleagues lose their life."
Read more: U.S., UK medics threatened to stay silent on lack of protective gear
Intensive workload, overwhelming mental stress
Nurses worldwide are also taxed beyond their physical limits as battling the pandemic.
Photos widespread on social media outlets showing health care staff exhausted after relentlessly long work hours.
In China, an early-March survey done by GZ Asclepius Healthcare, an independent third-party research organization on Chinese hospitals, showed that medical staff faced heavy workloads and their basic physical needs were difficult to meet during the early stage of the outbreak.
In the 9,883 questionnaires of medical staff from 25 provinces nationwide, medical staff worked an average of 8.15 hours a day during the outbreak, with 81.54 percent working even longer, and 5.67 percent more than 12 hours.
Frontline clinical medical workers needed to wear protective clothing, goggles, multi-layer masks and gloves, and they could drink, eat or going to the bathroom for as long as 5.2 hours, and the interval for 15.44 percent were as long as more than eight hours.
Meanwhile, when treating patients, they saw and heard a lot of negative information, such as pain and death. The infection or demise of their colleagues worsened their mental exhaustion.
The survey showed that many of them are fatigued, 21.21 percent moderately, 6.69 percent severely and 2.69 percent critically. Over 67.8 percent of medical workers had problem in their sleep quality, and 34.37 percent had moderate or more severe sleep disorder. Nearly 60 percent suffered tension, panic or fear.
China has issued a notice on the implementation of measures to further protect and care for medical workers both physically and psychologically.
"Without nurses, midwives, and other health workers, countries cannot win the battle against outbreaks, or achieve universal health coverage and the Sustainable Development Goals," cautioned WHO, calling on governments to "invest in a massive acceleration of nursing education, creation of nursing jobs, and leadership."
WHO: There is a global shortfall of 5.9 million nurses
The WHO has released a new report called "The State of the World's Nursing 2020," which outlines vital gaps in the nursing workforce and propriety areas for investment in nursing education, jobs, and leadership.
According to the report, nursing is the largest occupational group in the healthcare sector, which accounts for roughly 59 percent of health professions while provides important services throughout the whole health system. However, there are no more than 28 million nurses worldwide, about 5.9 million short of what the world needs to care for the increasing population now.
Amid the COVID-19 crisis, nurses show an irreplaceable status in the world. Nothing that 90 percent of nurses are female but few nurses or women hold leadership positions, WHO officials suggest leaders from across the globe should also strengthen the role of nurses in care times in the future.