Editor's note: On March 12, 2020, the World Health Organization (WHO) declared COVID-19 a pandemic, and as of Monday (April 20), about 200 countries and regions have confirmed over 2,245,000 cases, according to the WHO. On CGTN's live program "COVID-19 Frontline," we invited medical workers and experts from China's epicenter Wuhan and from all over the world to share their experiences and take questions from social media, in the hope of providing more information for those who are battling against the pandemic.

In the latest episodes of CGTN's live stream program "COVID-19 Frontline," Chinese frontline doctors, including Shang You, Director of Critical Care Medicine Department of Wuhan Jinyintan Hospital and Peng Zhiyong, Chair of Critical Care Medicine of Zhongnan Hospital of Wuhan University, share their experience of dealing with the coronavirus pandemic with counterparts from Canada, United States and Israel.
Live: Chinese doctors share first-hand experience in treating COVID-19 patients
Live: Chinese frontline doctors share COVID-19 treatment experience with Israeli medics
As of April 20, more than 155,000 people have died from COVID-19, the disease caused by SARS-CoV-2, in at least 185 countries and regions. Data shows 80 percent of patients have mild symptoms, meanwhile, 13.8 percent of cases suffer severe symptoms and six percent are critical.

Chinese doctors, who served on the front lines fighting against COVID-19 in Italy and Iran, share their experiences with their counterparts from Canada and U.S. via live stream program "COVID-19 Frontline." /CGTN
Chinese doctors, who served on the front lines fighting against COVID-19 in Italy and Iran, share their experiences with their counterparts from Canada and U.S. via live stream program "COVID-19 Frontline." /CGTN
The treatment of COVID-19 related cytokine storms
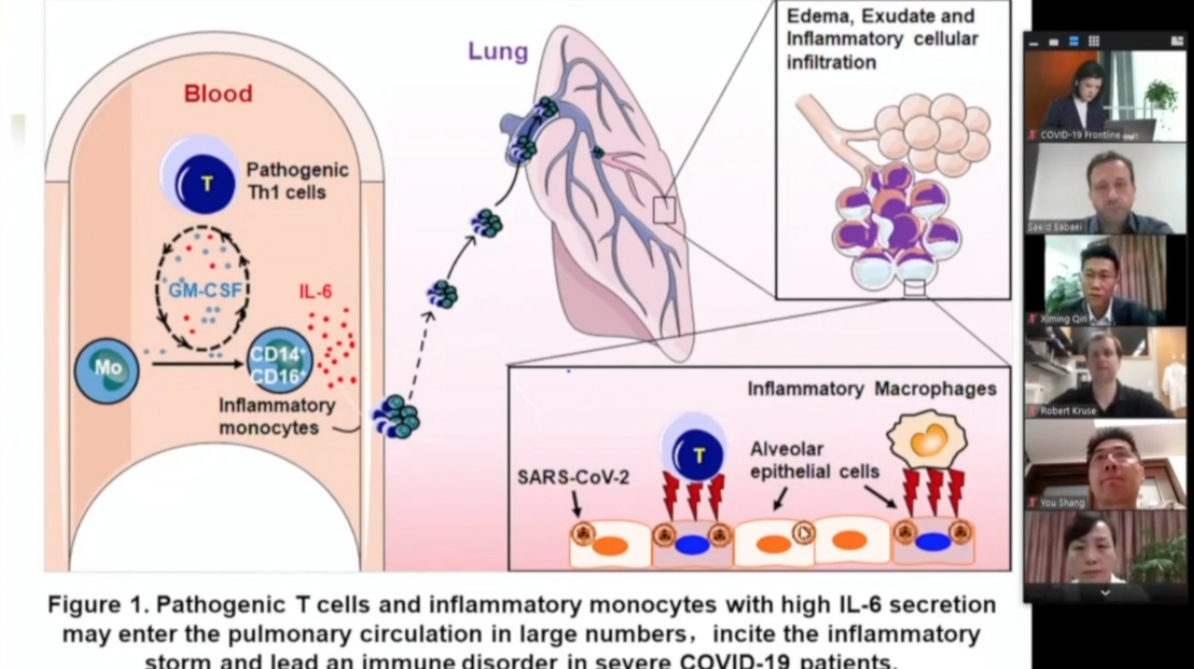
In some cases of COVID-19 the patients struggle through the first week of illness, then suddenly they crash. The crash can occur in healthy victims of COVID-19 as well. The problem, known as a "cytokine storm," happens when a person's own immune system overreacts to the virus and causes more damage to its own cells.
Saeid Babaei, an expert on antibody and Chairman & CEO of Virotek Inc., Canada, wanted to know the drugs that can help control the cytokine storm.
Fu Binqing, professor of Immunology at the University of Science and Technology of China, introduced Tocilizumab treatment to reduce mortality of severe COVID-19.
Tocilizumab calms the inflammatory storm through blocking IL-6 receptors. According to Fu, 21 patients diagnosed as severe of critical COVID-19 were given Tocilizumab in addition to routine therapy between February 5 and 14, and 19 of those 21 patients were discharged on average 13.5 days after receiving the treatment. In addition, the immunotherapy strategy about Tocilizumab treatment has been formally included in the diagnosis and treatment program of COVID-19 (7th edition) of the National Health Commission of China.
05:59
Is convalescent plasma effective in treating COVID-19?
In the guidelines on the diagnosis and treatment of the virus, China's health authorities said plasma of recovering patients could be employed to fight COVID-19. Saeid Babaei wanted to know about the practical experience related to the therapy.
Dr. Shang You confirmed the effectiveness of the convalescent plasma in treating COVID-19 patients. According to the guidelines on convalescent plasma treatment issued by China's National Health Commission, the therapy should be used on patients who have severe or critical conditions. Although it's not easy to find donors who meet certain criteria, and there are some complications. But since there is no wonder drug for COVID-19 yet, convalescent plasma is still useful.
Suggestions about intubation and mechanical ventilation
02:31

Dr. Jameel Mohsen from Israel is concerned about the safety of intubation and when should it be used.
Hu Bo, Vice-Director of Critical Care Medicine of Zhongnan Hospital of Wuhan University, recommended early intubation to reduce lungs damage. The invasive mechanical ventilation treatment should be implemented as soon as possible, when a patient's oxygenation index is ≤150 mmHg.
Besides, prone position is suggested to better protect the lungs, although it takes two to three hours to see the improvement of oxygenation, added Dr. Peng Zhiyong, who led two ICU teams of more than 170 medics at Wuhan's Leishenshan Hospital.

Chinese doctors share COVID-19 treatment experience with medics from Israel via conference call. /CGTN
Chinese doctors share COVID-19 treatment experience with medics from Israel via conference call. /CGTN
Biomarkers of myocardial inflammation
Dr. Elias Hellou from Israel is concerned about cardiovascular comorbidities, a major risk factor for severe patients with COVID-19.
Dr. Peng said troponin is an important marker, and whether the heart muscle contracts or not. The other thing is acute pulmonary inflammation, because the left side of the heart is inhibited, it suppresses the blood flow, so if the function of the left atrium is improved, hypoxemia can be solved. Acute pneumonia should also be considered.
In later episodes of "COVID-19 Frontline," more frontline doctors and experts from Wuhan will join in to share their experience with their colleagues from other parts of the world. If you have any questions regarding COVID-19, you can share with us using #MyOpinionOnCOVID19 on Facebook.
Videos by Mi Xue
Cover image by Du Chenxin