Editor's note: On March 12, 2020, the World Health Organization (WHO) declared COVID-19 a pandemic, and as of Wednesday (April 22), about 200 countries and regions have confirmed over 2,475,000 cases, according to the WHO. On CGTN's live program "COVID-19 Frontline," we invited medical workers and experts from China's epicenter Wuhan and from all over the world to share their experiences and take questions from social media, in the hope of providing more information for those who are battling against the pandemic.

In the latest episode of CGTN's live stream program "COVID-19 Frontline" held on Wednesday, April 22, CGTN invited Chinese nurses from the Second Affiliated Hospital of Zhejiang University School of Medicine to share their first-hand nursing and personal protection experience with their counterparts from the United States and Kenya.
Some of the nurses who participated in the program worked in the intensive care unit in hard-hit Wuhan for more than two months. Some of them have been fighting the pandemic in Zhejiang Province. In the program, they also mentioned some touching stories that happened in the wards.

Chinese nurses share COVID-19 working experience with their foreign counterparts. /CGTN
Chinese nurses share COVID-19 working experience with their foreign counterparts. /CGTN
According to China's National Health Commission, among the medical teams dispatched to support Wuhan, there are 42,000 medical workers, among whom 28,600 are nurses, accounting for 68 percent of the total. Their meticulous care has given the patients great help and support.
Live: Chinese frontline nurses share COVID-19 experience
How to protect frontline medical staff?
Theresa Brown, a nurse and best-selling author from the United States, wanted to know how do Chinese frontline healthcare workers keep safe from the coronavirus?
Song Jianping, associate director of Nursing Department, SAHZU head of SAHZU's Nursing Team in Wuhan, said that strictly wearing personal protective equipment is the most important barrier to prevent healthcare workers from getting infected. She and her team were working in the intensive care unit, so all medical staff needed to wear full protective equipment, including protective clothing, N95 masks, gloves, foot covers, goggles and so on.
06:37

During the dressing process, two medical staff are responsible in each shift to supervise whether the protective equipment of all nursing staff is in place and whether there are any omissions. In addition, when taking off protective clothing, it's required to have two nurses in pairs to supervise each other to make sure the procedure is correct.
Song also introduced that there are requirements for high-risk operations. For example, when performing endotracheal intubation, medical staff must wear positive pressure head-gear, the protection measures should be strengthened. In the ICU area, nurses are required to avoid gathering when passing their work on to the next shift.
How can healthcare workers avoid infecting family members?
Sheila Alexander, associate professor at School of Nursing and School of Medicine at the University of Pittsburgh, wanted to know how healthcare workers avoid infecting family members when they get home from work.
Jin Jingfen, director of Nursing Department, SAHZU member of the hospital's COVID-19 Response Steering Committee, and Song Jianping respectively answered the different standards for the areas outside Hubei Province and hard-hit pandemic areas including Wuhan.
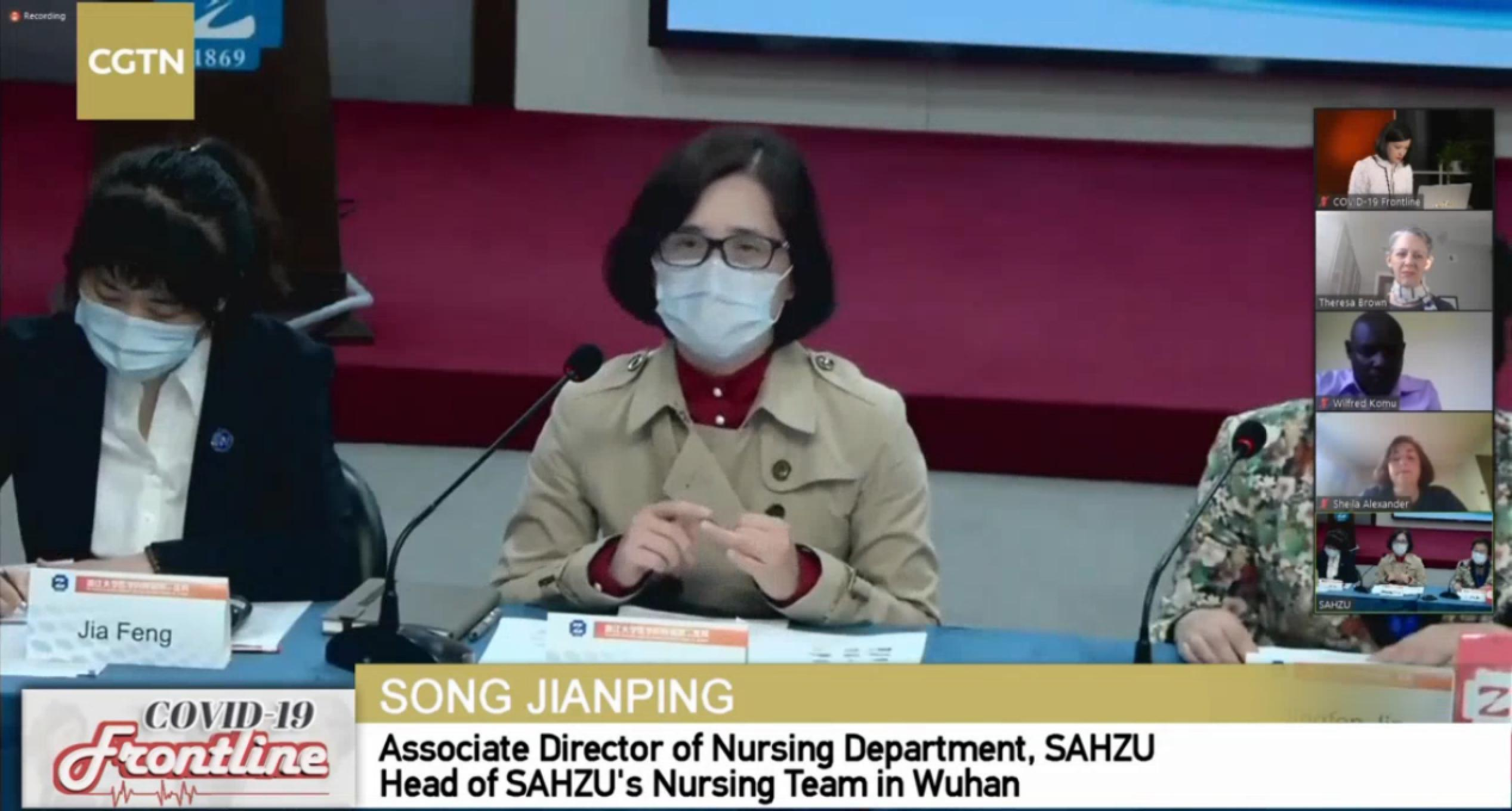
Song Jianping, Associate Director of Nursing Department, SAHZU Head of SAHZU's Nursing Team in Wuhan, shares her COVID-19 working experience. /CGTN
Song Jianping, Associate Director of Nursing Department, SAHZU Head of SAHZU's Nursing Team in Wuhan, shares her COVID-19 working experience. /CGTN
In non-high-risk areas, such as Hangzhou in Zhejiang Province, hospitals provide medical staff with sufficient disinfection materials such as alcohol disinfectant, masks, hand sanitizers and disinfectant wipes for them to fully disinfect in and out of the hospital, Jin said. When a medical staff gets home, he or she needs to take off coats, disinfect them, wash hands and wear masks.
In addition, the hospital requires the medical staff involved in the treatment of COVID-19 to report their body temperature, personal health status and their contact history. Medical workers can also apply to stay in hospital dormitories or hotels to avoid contact with family members.
In Wuhan and other hard-hit areas, medical workers needed to stay in completely isolated accommodations. According to Song Jianping, the medical staff lived in the hotel arranged by the government and they couldn't visit each other in order to avoid the spread of the virus. The catering and other daily needs were all provided by hotels.
Apart from this, monitoring the health status of people entering and leaving the community via QR codes is also an important means to prevent community transmission.
Advice on diagnostic process
Wilfred Komu, Clinician and Public Health Expert in Kenya, asked how Chinese hospitals design diagnostic systems and admission procedures to cope with COVID-19 outbreaks.
Jin Jingfen replied that strict management measures are an important means to prevent nosocomial infections. When a patient comes to the hospital, he or she will first receive the temperature check and health QR code check. If a patient with fever or suspected symptoms is found, he or she will be transferred to the fever clinic for examination.
The general fever ward should be distinguished from the suspected COVID-19 ward. Preliminary judgment is made through epidemiological history investigation, temperature check, blood test, CT scan and etc. Suspected patients with COVID-19 need to get nucleic acid test.
Usually, if the suspected patient tested negative for the first time, he or she will be admitted to the isolation ward and will be retested after 24 hours. All the confirmed COVID-19 patients will be sent to designated hospitals for further treatment.

CGTN's live stream program "COVID-19 Frontline." /CGTN
CGTN's live stream program "COVID-19 Frontline." /CGTN
Jin added that during the pandemic, patients who go to outpatient or emergency department also need to undergo epidemiological screening, and patients with suspicious symptoms will be sent to fever clinic for further examination. Besides, a special independent area is left ready for emergency rescue use.
How to support and take care of dying patients?
Sheila Alexander said since COVID-19 is an infectious disease, patients' families are often unable to visit and accompany them. Therefore, taking care of critically ill patients and giving them psychological support has become a challenge for American medical workers.
Wang Lizhu, head ICU nurse, SAHZU member of SAHZU's Nursing Team in Wuhan, said they also had the same situation. Nurses usually try to accompany patients through their final moments via companionship and communication, such as holding the patient's hand, letting them know that they are with them, or comforting the patient with words to let them feel that they are not alone.
05:50

Wang said doctors and nurses often try to meet patients' demands. She mentioned a nurse in her team once brought a chocolate to a patient who wanted one. Though it was only a little thing, it moved the patient deeply.
Wang added that nurses try to comfort patients as much as they can. She herself has called a patient's family members and asked them to record a message and then play it in that patient's ward. So the patient can hear his family at least in his last days of life.
"I don't know if the patient heard that, but I believe he can, and I believe he can see my eyes through the goggles and see us being around and encouraging him," Feng Xiuqin, associate director of the nursing department, SAHZU member of the hospital's COVID-19 Response Working Committee, said.
Asked how she felt about caring for COVID-19 patients, Feng said she was scared at first because she was facing a completely unknown virus.
"We are ordinary people, we also have family and friends, and wearing a three-layer protective suit can be very uncomfortable, heavy and sometimes painful, and it is difficult to do even the smallest actions," Feng said. "I remember a doctor crying in a hospital room because he couldn't give an injection, which is usually easy. Sometimes I feel powerless because I can't save the patient."
However, Feng said that after wearing the white protective suit and receiving encouragement from all walks of life, she became brave because of the support she gets, touched by the respect of the patients, and proud to be able to help save lives.
"I'm also proud that at this point, for example, we can share our experience with healthcare workers from around the world," she said.
In later episodes of "COVID-19 Frontline," more frontline doctors and experts from Wuhan will join in to share their experience with their colleagues from other parts of the world. If you have any questions regarding COVID-19, you can share with us using #MyOpinionOnCOVID19 on Facebook.
Videos by Zhang Rongyi
Cover image by Du Chenxin