
Editor's note: Henrietta H. Fore is executive director of the United Nations Children's Fund (UNICEF). Tedros Adhanom Ghebreyesus is director-general of the World Health Organization. Natalia Kanem is executive director of the United Nations Population Fund. Kevin Watkins is CEO of Save the Children UK. The article reflects the authors' opinions and not necessarily the views of CGTN.
As the world focuses its attention on winning the battle against COVID-19, we must not forget that we are still fighting a war against preventable child and maternal deaths – a war that world leaders pledged to win by 2030. The international community must recommit to that promise and deliver on it this decade.
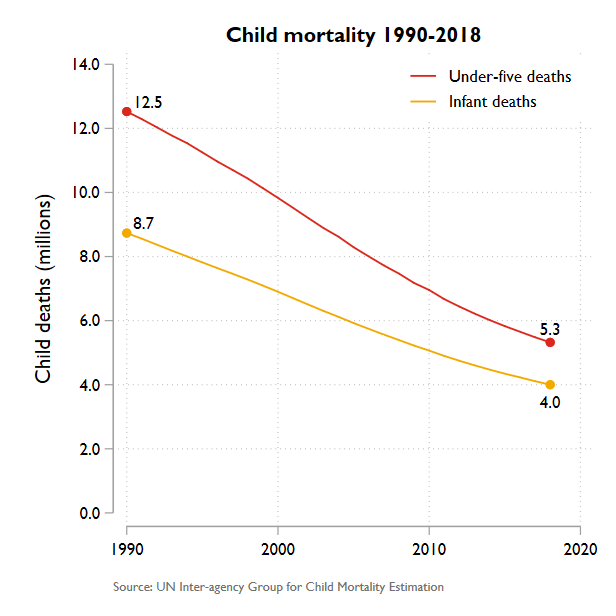
Child survival is perhaps the greatest untold success story in the recent history of international development. Since the early 1990s, the mortality rate for children under age five has plunged by nearly 60 percent. And the annual rate of decline has accelerated since 2000, saving millions of lives. Maternal mortality has also fallen rapidly – by nearly 40 percent over the last 20 years.
These gains are largely the result of efforts to extend the reach of health systems in the world's poorest countries. Primary health care has been the catalyst for some of the most impressive gains. Countries such as Bangladesh and Ethiopia have achieved astonishing progress by training and deploying health workers where they can be most effective – namely, in the communities they serve.
International cooperation has been another powerful driver of change. Aid provided through Gavi, the Vaccine Alliance since 2000 has enabled over 760 million people to be immunized against deadly diseases, saving more than 13 million lives.
Despite this progress, children and their mothers are still dying at appalling rates. Over five million young lives are still being lost every year – almost half in the first month of life – to preventable or treatable diseases like pneumonia, malaria, and diarrhea. More than 800 women and adolescent girls die every day from preventable causes related to pregnancy and childbirth, owing largely to a lack of reproductive health care.
Even before the COVID-19 pandemic, the world was not on track to deliver on its promise – included in Sustainable Development Goal 3 – to end preventable maternal and child mortality by 2030. If progress over the next decade mirrors the last, over three million children will still be dying annually in 2030. Maternal survival goals will also be missed by a wide margin.
The danger now is that COVID-19 will widen the gap between the SDG promise and reality. Supply-chain disruptions, intensifying financial pressures, and the diversion of health workers and resources are already undermining service delivery in vulnerable areas. Gavi reports delays on "14 Gavi-supported immunization campaigns," as well as "four national vaccine introductions," leaving over 13 million people – many of them children – without vaccine protection.
A chart provided by Project Syndicate
A chart provided by Project Syndicate
Meanwhile, lockdown policies and fear of infection are deterring people from seeking other kinds of health care. Researchers at the Johns Hopkins University School of Medicine estimate that a 15 percent reduction in the use of routine health services over a six-month period could lead to an additional 253,000 child deaths. Another research team at the Guttmacher Institute estimates that even a modest decline of 10 percent in coverage of pregnancy-related and neonatal health care would result in an additional 28,000 maternal deaths and 168,000 newborn deaths.
We have seen this story play out before. During the 2014-16 Ebola crisis in West Africa, the breakdown in routine service delivery caused a catastrophic surge in child deaths from malaria and other diseases, as well as an increase in maternal mortality and stillbirth.
Like Ebola, COVID-19 demands the world's attention – and cooperation. Without a vaccine, there is no exit from the pandemic. That is why the development and equitable distribution of a vaccine is so critical. International cooperation to strengthen health systems and deliver the tests, protective equipment, and medical supplies needed to save lives remains a first-order priority.
But we must not allow a new health crisis, however deadly, to increase the toll of old killers on the world's most disadvantaged children and women. Avoiding that outcome will require a four-pronged approach.
First, governments and aid donors must defend hard-won gains in child and maternal health by protecting budgets for community health services, including maternal health care and immunization. Next month's donors' meeting to decide on Gavi's funding for 2021-25 is critical. By heeding Gavi's call for 7.4 billion U.S. dollars in funds, donors would enable the organization to immunize an additional 300 million children in developing countries over this period – saving up to eight million lives. There is no more cost-effective health investment.
Second, efforts to build more resilient health systems should be strengthened, with a focus on addressing the weaknesses that COVID-19 has exposed. For example, many of the world's poorest countries lack medical oxygen, which is essential for treating not only COVID-19, but also childhood pneumonia – which kills 800,000 under-five children each year – as well as malaria, sepsis, and newborn respiratory problems.
Third, it is time to abandon the false notion that universal health coverage is an unaffordable luxury. What is unaffordable is the inequality, suffering, and inefficiency that comes with financing health services through user charges imposed on people too poor to pay. With poverty set to rise, the elimination of these charges and strengthening of publicly financed health systems is more urgent than ever. In fact, universal health coverage is included in the same SDG as preventable maternal and child deaths, underscoring their interconnectedness.
Finally, as financial pressures on health systems mount, we must explore every avenue for resource mobilization. The International Monetary Fund and the World Bank have secured a commitment from the G20 countries to suspend debt repayment from the poorest countries. Surely this is an opportunity to convert money earmarked for debt servicing into an investment fund for child and maternal health.
COVID-19 is a devastating reminder of our shared vulnerability. But we are all united by the shared values reflected in our pledge to end preventable child and maternal deaths. As we fight the pandemic, we must hold to that pledge and fulfill the promise made to the children and women whose lives are at stake.
Copyright: Project Syndicate, 2020.
(If you want to contribute and have specific expertise, please contact us at opinions@cgtn.com.)