Editor's note: On March 12, 2020, the World Health Organization (WHO) declared COVID-19 a pandemic, and as of Wednesday ( June 10), about 200 countries and regions have confirmed over 7,039,000 cases, according to the WHO. On the CGTN live program "COVID-19 Frontline," we invite medical workers and experts from China and other parts of the world to share their experiences and take questions from social media, in the hope of providing more information for those who are battling the pandemic.
In the latest episode of CGTN's live stream program "COVID-19 Frontline" held on Tuesday, June 9, CGTN invited four prominent health experts from Peking University Third Hospital, one of the top hospitals under China's National Health Commission, to share their treatment strategies with peers from Brazil.
Live: China's top medics share COVID-19 treatment experience with Brazilian peers
Qiao Jie, an academician at the Chinese Academy of Engineering and president of Peking University Third Hospital, said more than 400 medical workers from the hospital were dispatched to Wuhan to fight against the epidemic and worked continuously for more than 70 days. The medics have accumulated a lot of experience in epidemic control, patient examination and treatment. Qiao said it is also a duty to share these experiences with the world.
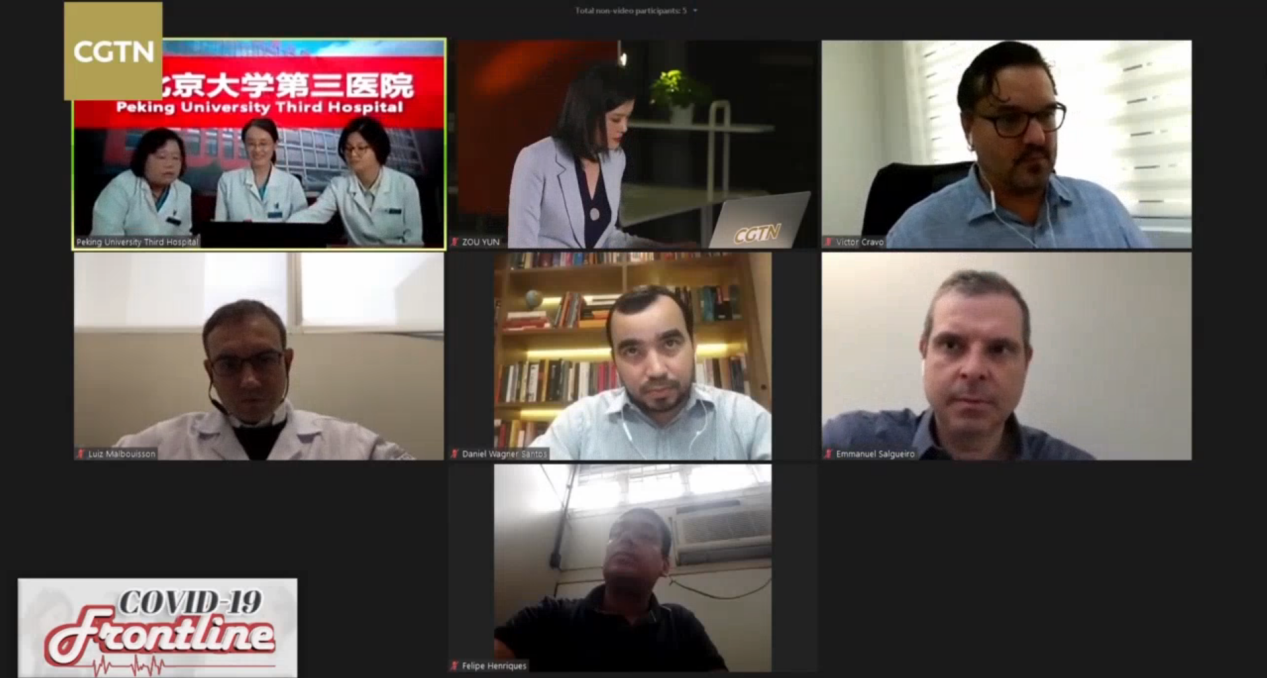
CGTN's live stream program "COVID-19 Frontline" held on June 9, 2020. /CGTN
CGTN's live stream program "COVID-19 Frontline" held on June 9, 2020. /CGTN
Brazil has seen a continuous spike in COVID-19 deaths over the past few weeks. The number of COVID-19 cases in Brazil totals 739,503 with 38,406 deaths, according to the Johns Hopkins University COVID-19 dashboard. So far the country has the second highest number of infections in the world, after the U.S.
How to reduce the ICU mortality rate
Victor Cravo, head of medical management of the ICU at Americas Medical Services, said the mortality rate of patients receiving mechanical ventilation is high in both public and private services in Brazil. So he wanted to know the experience of Chinese doctors and if there is any different approach to managing the patients.
Li Shu, attending physician of Emergency Medicine, Peking University Third Hospital, answered that they also had a high mortality rate at the beginning when ICU mortality rate was around 52 percent, similar to the rate in Brazil today.
"At the beginning, there were too many patients waiting to be admitted in Wuhan, and we lacked medical equipment. I think some patients developed very quickly in the early stage, so the high mortality rate was normal at the beginning," Li said. But later with enough equipment to treat patients, the mortality rate got lower.
03:52

The role of glucocorticoid in COVID-19 treatment
Victor Cravo also asked about the use of glucocorticoid in the treatment of COVID-19 patients.
Shen Ning, vice president of Peking University Third Hospital and professor of pulmonary and critical care medicine, said they did use glucocorticoid to treat COVID-19 patients. It's a common anti-inflammatory drug that is used to treat other coronavirus infections such as SARS (severe acute respiratory syndrome) and MERS (Middle East respiratory syndrome), but it's still controversial as it may cause sequelaes of varying degrees.
"We used some glucocorticoid in some critically ill COVID-19 patients," Shen said. "We need to use it very cautiously, especially on patients with underlying diseases including diabetes and hypertension, or who have fungal or bacterial infections. The recommended dosage of glucocorticoid is also low."

Doctors from Peking University Third Hospital. /CGTN
Doctors from Peking University Third Hospital. /CGTN
The use of heparin
Luiz Malbouisson, professor of anesthesiology at University of the Sao Paulo Medical School, said 40 percent of patients have microthrombi in the lungs. So he wanted to know about Chinese doctors' experience in using heparin.
Li Shu said among the patients they treated, some had elevated D-dimer, and one or two patients had other clotting indicators. They used low molecular weight heparin (LMWH) and heparin with non-standard doses, but for patients with confirmed thrombus, full dose of heparin was applied. Study shows heparin can effectively reduce the death rate in severe and critical patients with elevated D-dimer, according to Dr Li.
CGTN's live stream program "COVID-19 Frontline." /CGTN
CGTN's live stream program "COVID-19 Frontline." /CGTN
When can patients be discharged from hospital?
Daniel Wagner Santos, an infectious disease consultant of Sao Luiz Hospital, asked about the IgM and IgG tests and when can patients be discharged from hospital.
Li Chao, attending physician of critical care medicine at Peking University Third Hospital, said IgM is generally detected within 3 to 5 days after the onset of illness, and the patient needs to receive a serological test before discharge to determine whether he or she is fully recovered.
Li Shu added that there are three main requirements for patients to be discharged from hospital. The first is that their body temperature needs to remain normal for three consecutive days; the second is that their lung symptoms improve, and the third is that their PCR tests are negative for two consecutive days. She added that after being released from the hospital, the patient still needs to undergo 14 days of isolation and two more PCR tests.
02:10

In later episodes of "COVID-19 Frontline," more frontline doctors and experts from Wuhan will join in to share their experience with their colleagues from other parts of the world. If you have any questions regarding COVID-19, you can share them with us using #MyOpinionOnCOVID19 on Facebook.
Videos by Zeng Hongen
Cover image by Du Chenxin