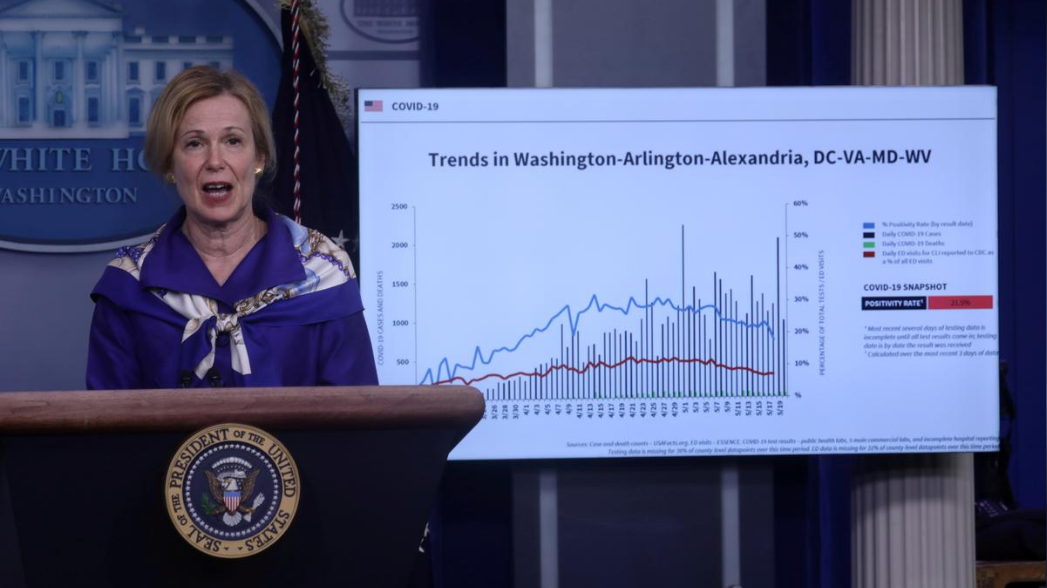
Dr. Deborah Birx, the White House coronavirus response coordinator, addresses a news conference about the pandemic at the White House in Washington, the U.S., May 22, 2020. /Reuters
Dr. Deborah Birx, the White House coronavirus response coordinator, addresses a news conference about the pandemic at the White House in Washington, the U.S., May 22, 2020. /Reuters
The United States is in a new phase of the novel coronavirus outbreak with infections "extraordinarily widespread" in rural areas as well as cities, White House coronavirus experts said on Sunday as COVID-19 cases continue to surge in some parts of the country and medical experts began to study possible long-term costs.
"We are in a new phase," said Dr. Deborah Birx. "What we are seeing today is different from March and April," Birx told CNN's "State of the Union," adding that the pandemic was affecting both urban and rural areas.
"To everybody who lives in a rural area: You are not immune or protected from this virus," Birx said.
Birx, the White House task force coordinator, said people living in multigenerational households in an area that is experiencing an outbreak should wear masks inside the home to protect the elderly or those with underlying conditions.
Admiral Brett Giroir, an assistant Health and Human Services secretary, continued to stress the importance of wearing masks.
"If we don't do that, and if we don't limit the indoor crowded spaces, the virus will continue to run," he said on NBC's "Meet the Press."
"We are very concerned and this is a very serious point."
Birx said what she witnessed as she visited 14 states over the last three weeks gave her cause for concern.
"As I traveled around the country, I saw all of America moving," Birx said. "If you have chosen to go on vacation into a hot spot, you really need to come back and protect those with comorbidities and assume you're infected."
So far, the coronavirus has infected about 4.6 million people in the U.S. and killed more than 155,000 Americans. Medical experts have warned that their work on the front line will be in vain if the country can't contain the surging coronavirus cases.
According to a recent study published by The Lancet Public Health journal, front-line healthcare workers in the UK and the U.S. were over three times more likely to test positive for the coronavirus compared with the general community.
WHO on Friday announced that at least 10 percent of all global COVID-19 cases are among health workers. During a press briefing, Tedros Adhanom Ghebreyesus, WHO chief said "we all owe health workers an enormous debt. Not just because they have cared for the sick, but because they have risked their own lives in the line of duty."

Laura Gross rests on her balcony in Fort Lee, New Jersey, the U.S., July 31, 2020. /Reuters
Laura Gross rests on her balcony in Fort Lee, New Jersey, the U.S., July 31, 2020. /Reuters
Long-term costs of COVID-19
Aside from overwhelmed health systems and health workers, medical experts are also concerned about the long-term economic and health toll of the coronavirus as studies of COVID-19 patients keep uncovering new complications associated with the disease and mounting evidence show some COVID-19 survivors may face months or possibly years of debilitating complications.
Laura Gross, 72, had a gall bladder surgery in late March and became sick again when she was recovering from the surgery. Her throat, head and eyes hurt, her muscles and joints ached and she felt like she was in a fog. Her diagnosis was COVID-19. Four months later, these symptoms remain.
A JAMA Cardiology study found that in one group of COVID-19 patients in Germany aged 45 to 53, more than 75 percent suffered from heart inflammation, raising the possibility of future heart failure.
A Kidney International study found that over a third of COVID-19 patients in a New York medical system developed acute kidney injury, and nearly 15 percent required dialysis.
Dr. Marco Rizzi in Bergamo, Italy, an early epicenter of the pandemic, said the Giovanni XXIII Hospital has seen close to 600 COVID-19 patients for follow-up. About 30 percent have lung issues, 10 percent have neurological problems, 10 percent have heart issues and about nine percent have lingering motor skill problems. He added that even those with mild COVID-19 "may have consequences in the future."
Healthcare experts say it will be years before the costs for those who have recovered can be fully calculated. The costs stem from COVID-19's toll on multiple organs, including heart, lung and kidney damage that will likely require costly care, such as regular scans and ultrasounds, as well as neurological deficits that are not yet fully understood.
Bruce Lee of the City University of New York (CUNY) Public School of Health estimated that if 20 percent of the U.S. population contracts the virus, the one-year post-hospitalization costs would be at least 50 billion U.S. dollars, before factoring in longer-term care for lingering health problems. Without a vaccine, if 80 percent of the population became infected, that cost would balloon to 204 billion U.S. dollars.
In the U.S., more than half of the population is covered by private health insurers. Lee estimated the average one-year cost of a U.S. COVID-19 patient after they have been discharged from the hospital at 4,000 U.S. dollars, largely due to the lingering issues from acute respiratory distress syndrome (ARDS), which affects some 40 percent of patients, and sepsis.
The estimate spans patients who had been hospitalized with moderate illness to the most severe cases, but does not include other potential complications, such as heart and kidney damage. Even those who do not require hospitalization have average one-year costs after their initial illness of 1,000 U.S. dollars, Lee estimated.
(With input from Reuters)