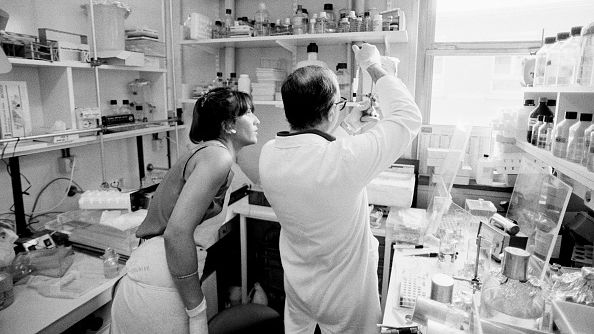
Luc Montagnier (R), one of the people who identified the virus that causes AIDS in 1983, is pictured in his lab with a colleague at the Institut Pasteur in Paris, France, August 1987. /Getty
Luc Montagnier (R), one of the people who identified the virus that causes AIDS in 1983, is pictured in his lab with a colleague at the Institut Pasteur in Paris, France, August 1987. /Getty
On June 5, 1981, an article in a U.S. medical publication detailed the cases of five young men in Los Angeles: all were gay, around the same age, sexually active and all had a rare disease usually seen only in people whose immune system was exceptionally weak.
It was the first report about what would later become known as HIV/AIDS and it was soon followed by similar dispatches from around the country and abroad.
Over the next 40 years, HIV/AIDS would become one of the biggest health crises in the world, killing millions.
But how it was discovered amounted almost to chance, according to one of the doctors who authored the first report.
'Whatever he's got, the other guy's got it too'
Andy Saxon was 35 years old and an associate professor of medicine and chief of clinical immunology/allergy at UCLA Medical School.
"In 1980, an intern brought to the attention of my colleague and me, a young man who had pneumocystis carinii pneumonia (PCP)," Saxon told CGTN via Skype from Los Angeles. "And that was very unusual because PCP is a disease of the very immunocompromised: really immunocompromised people get this infection, otherwise you can fight it off."
"So it's weird but it's a one-off."
A few months later however, Saxon and his colleague Michael Gottlieb met another patient with a severe candida growth on his finger – "the kind of infection you never see in people who aren't really immunocompromised."
"I looked at Mike and Mike looked at me and said, 'Whatever he's got the other guy's got it too.' So now there's two, it's no longer a one-off. And that was the beginning."

A 1986 photo of the clinical immunology/allergy group at UCLA Medical School, with Michael Gottlieb (in a blue shirt) and Andy Saxon (in a yellow shirt) in the center, in the tree. /Photo courtesy of Andy Saxon
A 1986 photo of the clinical immunology/allergy group at UCLA Medical School, with Michael Gottlieb (in a blue shirt) and Andy Saxon (in a yellow shirt) in the center, in the tree. /Photo courtesy of Andy Saxon
Gottlieb started digging around and found three more cases: these would be the five mentioned in the article published in the U.S. Centers for Disease Control and Prevention's (CDC) Morbidity and Mortality Weekly Report (MMWR) in June 1981.
But it was still unclear what these patients had. All five men had been previously healthy, but they now variously experienced long bouts of fever, shortness of breath, extreme weight loss and lesions.
"We thought 'we don't know what it is but clearly it seems to be in gay men'," Saxon recalled. The five were all gay and sexually active and they all had, or had had, a cytomegalovirus (CMV) infection, which is sexually transmitted. "It seemed logical that there was an infectious agent that was being sexually transmitted," said Saxon.
Given who seemed to be contracting the disease, it was initially called GRID, or gay-related immune deficiency – a term that would be unthinkable nowadays. "Today we would be pilloried for it," Saxon admitted.
'It didn't dawn on me'
It did not occur to the UCLA doctors that what they were seeing was the beginning of a global public health crisis.
"At the time it wasn't that dramatic. It was clearly something, but until the public health implications became more apparent, it was an oddity, not an emergency," noted Saxon.
The virus had been spreading for several years but people had not been falling seriously ill until then. "It didn't dawn on me, I didn't have a Eureka moment: 'Oh this is a huge problem'."

A volunteer speaks with an AIDS patient in hospital in San Francisco, U.S., November 20, 1985. /Getty
A volunteer speaks with an AIDS patient in hospital in San Francisco, U.S., November 20, 1985. /Getty
Only when the CDC became involved and reports emerged around the country of similar cases among people who injected drugs, haemophiliacs (who had become infected via blood transfusions) and Haitians (HIV is now known to have reached the U.S. from Africa via Haiti), did it become clear that this was something big.
It took two more years after the MMWR article – which was followed by a more detailed report in The New England Journal of Medicine in December 1981 – for French researchers to finally identify the virus that causes AIDS.
By 1992, AIDS was the leading cause of death among young men in the U.S. A decade later, it was the main cause of death in Africa.
To date, 34.7 million people worldwide have died of AIDS-related illnesses, according to UNAIDS. Another 38 million still live with HIV.
Fortuitous findings
Two anecdotes illustrate just how much work was done by trial and error in those early days.
A UCLA colleague of Gottlieb and Saxon's, Howard Schanker, was doing research on T4 cells – white blood cells that fight infection and play an important role in the immune system – and offered to run some tests on their patients. Today, it is well known that T-cell counts drop dramatically in AIDS patients, but in 1981, the doctors were shocked to find they were absent in the five men.
"That was a really key piece of data that was really dramatic," said Saxon. But it was done purely on a whim. "I use that as an anecdote of how science progresses by accident, by fortuitous findings," he said.

Teenagers receive counseling before testing for HIV at the Naguru Teenage Health Centre in Kampala, Uganda, May 23, 2005. /Getty
Teenagers receive counseling before testing for HIV at the Naguru Teenage Health Centre in Kampala, Uganda, May 23, 2005. /Getty
More frighteningly, the doctors did not realize at first that the disease was blood-borne. While performing a lung biopsy on one of the first patients, they did not wear gloves – "just to show you how naive we were!" Saxon recalled. A few years later, as it became clear that it was blood-borne, "there were some anxious moments," he admitted. "We had been less than careful."
No longer a death sentence
Things have changed dramatically since then. People with HIV can now live long lives thanks to antiretroviral combination therapy and may never get sick. But it wasn't always so.
"In the first 10 years, HIV was a death sentence. All the patients died, there was no recovery... it was frightening," Saxon noted.
Much like with COVID-19, there were also many people, including experts, who said it was all fake, that the virus did not exist.
Meanwhile, the expectation was that a vaccine would be found within 10 years. Four decades later, there is still no cure.
"HIV is the greatest shape-changer anyone has ever seen," noted Saxon. There are reportedly more mutant strains of HIV in a single patient with HIV than there are strains of influenza circulating around the world. This has made it immensely difficult to find an effective treatment, let alone a vaccine.

A cocktail of premixed AIDS drugs is shown in Miami, Florida, July 11, 2002. /Getty
A cocktail of premixed AIDS drugs is shown in Miami, Florida, July 11, 2002. /Getty
'Thinking outside the box'
Forty years on, Saxon credits "thinking outside the box" for his and his colleagues' 1981 find.
"Doctors are meant to put things in boxes. You're taught: here are the known diseases, here are the shapes, put round pegs in round holes, square pegs in square holes. You don't think outside the box." As academic immunologists, Gottlieb and him were more used to "seeing strange things."
But a lot of it also came down to chance and having two cases walk through UCLA's doors: other doctors had probably seen isolated cases but had dismissed them as one-offs.
"We just happened to see a little cluster... when you only see one, the lightbulb doesn't go off."
The UCLA doctors' report marked the first official recording of the HIV/AIDS epidemic, but if they hadn't spotted this new virus, somebody else would have, he insists.
Saxon, now emeritus professor and emeritus chief of clinical immunology/allergy at UCLA, did not continue working on HIV/AIDS, instead sticking to another field of immunology that he was already involved in. But he says he is impressed by the work that others did after him, even if mistakes were inevitably made along the way.
"They still don't have a vaccine… but they've got these antiretrovirals, these people are living long now.
"It took time but it was a whole uncharted territory."

