
Health
14:10, 09-Jul-2018
Smart bandages offer hope to those with persistent wounds
Updated
13:13, 12-Jul-2018
CGTN
A small cut or scrape may not worry you too much – we usually clean the wound, then bandage it and let the skin repair itself. But for persistent wounds, especially those suffered by diabetic patients, proper medical treatment is necessary otherwise bacterial infections will make things worse.
Tufts University in Massachusetts, the US, says a recent experiment has led to the creation of smart bandages, which make chronic wound healing less dangerous. Pre-clinical studies are ongoing but the bandages work in lab settings.
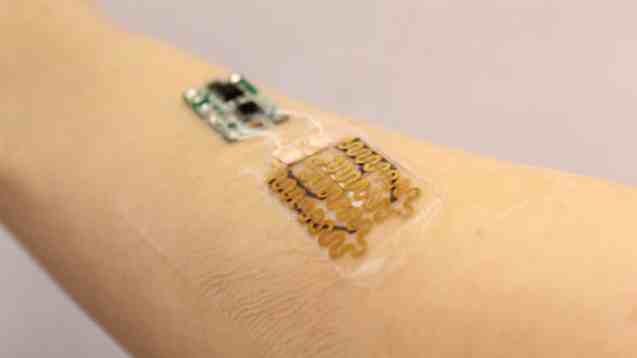
it might look like a bandage, but according to the research team, it is more of a wearable medical device.
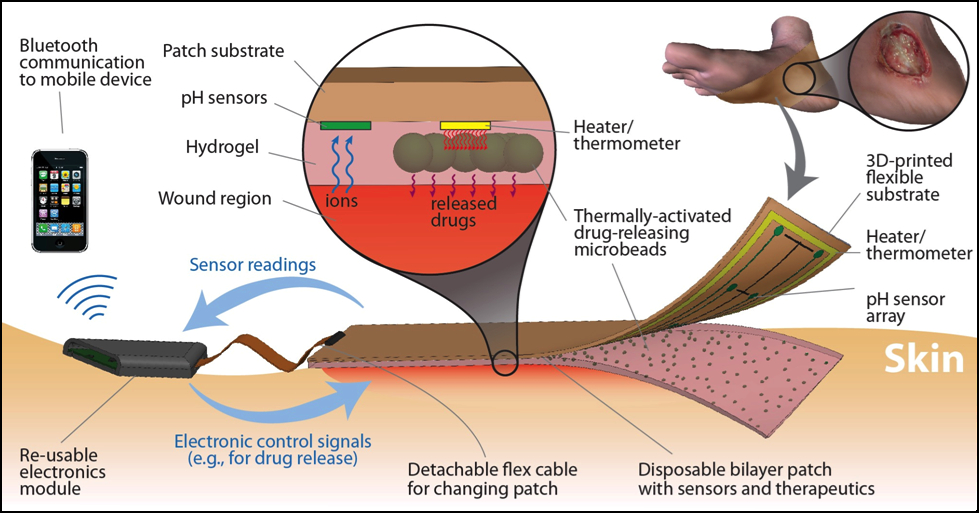
A detailed drawing shows the working process of the smart bandage designed. /Tufts University Photo
A detailed drawing shows the working process of the smart bandage designed. /Tufts University Photo
The device consists of two parts: One patch covers the wound, and the other reads data and sends signals to release drugs if necessary. In the patch are embedded pH and temperature sensors to monitor the healing process, including the level of inflammation in and around the wound.
When the patch collects information, the controller linked to it makes decisions about if antibiotics are needed, and if so, how much will be appropriate. Then, by heating thermally-activated microbeads within the patch, the correct amount of drug will be released.
In order to make the bandage cheaper and reusable, the research team used 3D-printed materials and detachable layers.
Professor Sameer Sonkusale, the co-author of the study, said that prototype is open to “a wide range of possibilities” since it different sensing components and drugs can be equipped, allowing the bandage to deal with different healing problems.
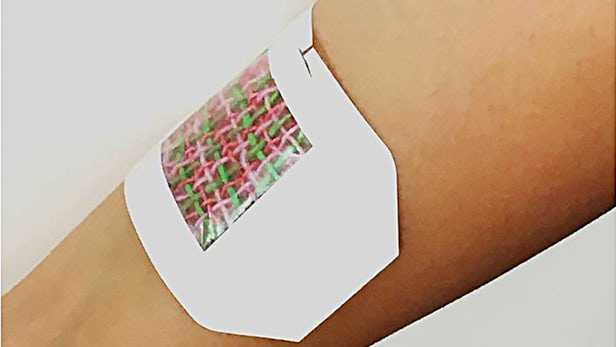
A prototype of the "wired" bandage designed by researchers from the University of Nebraska-Lincoln, Harvard Medical School and MIT /University of Nebraska-Lincoln Photo
A prototype of the "wired" bandage designed by researchers from the University of Nebraska-Lincoln, Harvard Medical School and MIT /University of Nebraska-Lincoln Photo
A similar device that can medicate wounds as needed was tested last October. Co-designed by researchers from the University of Nebraska-Lincoln, Harvard Medical School and Massachusetts Institute of Technology (MIT), it applied the same principle but used interwoven electrical fibers to heat a drug-releasing gel instead of using microbeads.
(Top image: A smart bandage attached to a human arm. The wound covering component (R) contains sensors and a drug carrier, and the microprocessor (L) interprets sensor input and triggers drug delivery. /Tufts University Photo)

SITEMAP
Copyright © 2018 CGTN. Beijing ICP prepared NO.16065310-3
Copyright © 2018 CGTN. Beijing ICP prepared NO.16065310-3