The recent COVID-19 outbreak has put the family of coronavirus under the spotlight. First found in the 1960s, coronaviruses have caused some major epidemics in the 21st century, including 2003's SARS (severe acute respiratory syndrome), 2012's MERS (Middle East respiratory syndrome) and the current COVID-19 outbreaks.
Among the three, MERS is known for its highest fatality rate of 34.3 percent, compared to 10 percent with SARS and 3.3 percent with COVID-19. Considering there is currently no vaccine available for the disease, finding the reservoir of MERS coronavirus (MERS-CoV) is perhaps the best way to prevent the disease from spreading.

Facts on MERS. /CGTN Graphic by Liu Shaozhen
Facts on MERS. /CGTN Graphic by Liu Shaozhen
To date, most MERS cases either took place in the Arabian Peninsula or had a history of traveling to countries in and nearby the region. Since 2012, MERS has spread to 27 countries, and nearly 80 percent of cases have occurred in Saudi Arabia, where the current MERS outbreak is taking place.
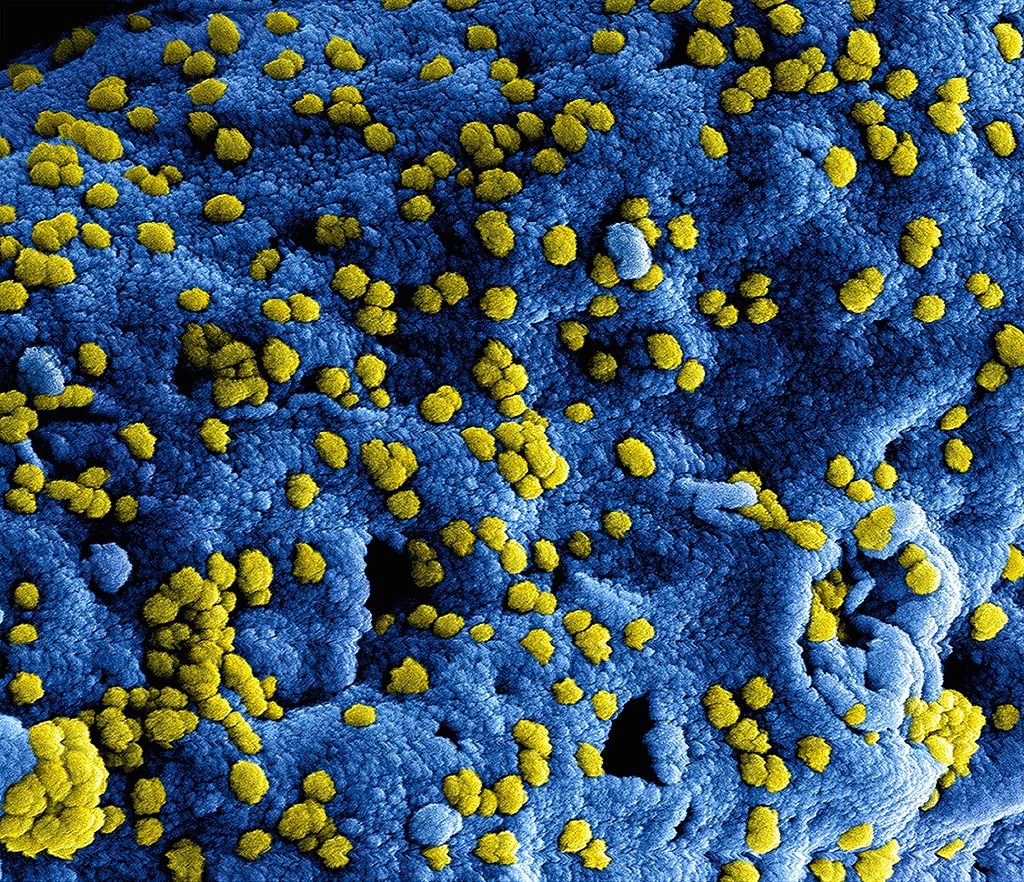
Numerous MERS-CoV viral particles (yellow) on the surface of a Vero E6 cell (blue). /VCG
Numerous MERS-CoV viral particles (yellow) on the surface of a Vero E6 cell (blue). /VCG
The dromedary camels in the Middle East, Africa and parts of South Asia soon became the main suspected reservoir of MERS-CoV as antibodies to MERS-CoV were detected in camel sera, indicating camels have been previously exposed to the virus.
In November 2013, a 43-year-old man who owned nine dromedary camels was infected with MERS-CoV. Before he showed symptoms, four of his camels were sick. Later, MERS-CoV viruses detected in him and the dromedary camel were found to be genetically identical, which further supports that dromedary camels are a potential host of the virus.

Two dromedary camels. /VCG
Two dromedary camels. /VCG
Unlike infected humans who might have fever, cough or even diarrhea and nausea, dromedary camels only show minor clinical signs after infection. Maybe that's why dromedary camels from the Middle East and Africa can harbor MERS-CoV for nearly 37 years without being noticed.
The earliest evidence of MERS-CoV in dromedary camels lied in camel serum samples collected from Somalia and Sudan between 1983 and 1984 and from Egypt in 1997. Among 189 samples, 81 percent were detected to have antibodies to MERS-CoV.
As of April 2018, serological evidence of MERS-CoV in dromedary camels has been found in 20 countries, mainly in the Arabian Peninsula and Africa. In another study, 550 camels in Kazakhstan, including 455 dromedary camels and 95 bactrian camels, were tested for MERS-CoV. All serum samples tested negative, showing that MERS-CoV was not present in camels in that region.

Two alpacas (Vicugna pacos). /VCG
Two alpacas (Vicugna pacos). /VCG
Besides dromedary camels, are there any other potential reservoirs of MERS-CoV? In a study conducted in Saudi Arabia between 2010 and 2013, serum samples of sheep, goats, cattle and chickens were collected from various regions, but all of them tested negative for MERS-CoV. Horse samples from UAE also tested seronegative.
However, researchers never gave up trying. In a research conducted in Qatar in 2015, 15 healthy alpacas who shared a barn with ten dromedary camels all tested seropositive to MERS-CoV, so did nine camels. The result suggested that alpacas are a potential reservoir of the virus. However, a previous research found no evidence of alpacas getting infected from other regions. More evidence is needed.

A dromedary camel in the desert. /VCG
A dromedary camel in the desert. /VCG
Despite all this evidence pointing dromedary camels as the reservoir of MERS-CoV, the exact transmission route is not fully understood. Given that there were coronaviruses isolated from bats that had a very close phylogenetic relationship to MERS-CoV, some suspected that the virus might have originated in bats and transmitted to dromedary camels at some unknown time, but it remained a hypothesis.
What we can do to prevent MERS-CoV might be to avoid contact with camels, not drink raw camel milk or eat undercooked camel meat as WHO recommends. Considering MERS-CoV RNA was found in the milk of infected camels, if you're a real lover of camel meat and camel milk, make sure they are fully cooked and pasteurized.
About 'Epidemics and Wildlife'
Nowadays, 70 percent of epidemics or pandemics are connected with wildlife. As humans continue to consume game meat and encroach on the habitat of wild animals, these viruses carried by them are more likely to be transmitted to humans. In this series, CGTN shows you how wildlife are connected with each epidemic such as Marburg and Ebola.
For more:
Are pangolins intermediate hosts of novel coronavirus?
How Nipah affects pig exports in Malaysia?
How are horses related to fatal Hendra virus?
How Ebola affects gorillas and chimpanzees?
How are African green monkeys linked to Marburg virus?
(Cover image via VCG, designed by CGTN's Du Chenxin.)
(If you want to contribute and have specific expertise, please contact us at nature@cgtn.com.)